Editor’s note: Discover the most recent COVID-19 news and assistance in Medscape’s Coronavirus Resource Center
.
Dealing with a yearlong siege from the coronavirus, the defenses in another, older war are failing.
For the last 20 years, HIV/AIDS has actually been held at bay by powerful antiviral drugs, aggressive screening and innovative public education projects. The COVID-19 pandemic has actually triggered extensive disturbances in nearly every element of that fight, grounding outreach groups, dramatically reducing screening and diverting crucial personnel away from labs and medical.
The specific effect of one pandemic on the other is still entering focus, however initial proof is troubling specialists who have actually commemorated the massive strides in HIV treatment. While the shift in concerns is across the country, hold-ups in screening and treatment bring especially severe dangers in Southern states, now the center of the country’s HIV crisis.
” This is a significant thwarting,” stated Dr. Carlos del Rio, a teacher of medication at Emory University in Atlanta and head of the Emory AIDS International Training and Research Study Program “There will be damage. The concern is, just how much?”
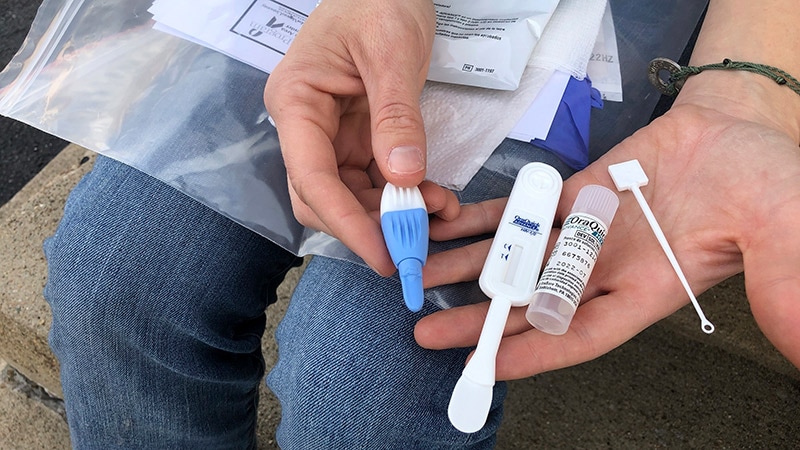
Centers have actually restricted in-person check outs and stopped regular HIV screening in physicians’ workplaces and emergency clinic, with doctors relying rather on video calls with clients, an useless option for those who are homeless or worry member of the family will find their status. Rapid-testing vans that when parked outdoors clubs and bars and given out prophylactics are mothballed. And, in state capitals and county seats, federal government knowledge has actually been singly concentrated on the all-hands-on-deck COVID action.
Concrete indications of the effect on HIV security are plentiful: One big business laboratory reported almost 700,000 less HIV screening tests throughout the nation– a 45%drop– and 5,000 less medical diagnoses in between March and September 2020, compared to the very same duration the year prior to. Prescriptions of PREPARATION, a preexposure prophylaxis that can avoid HIV infection, have actually likewise fallen dramatically, according to brand-new research study provided at a conference last month. State public health departments have actually tape-recorded likewise high decreases in screening.
That scarcity in brand-new information has actually caused a precarious, unknowable minute: For the very first time in years, the country’s admired HIV monitoring system is blind to the infection’s motion.
No place will the absence of information be felt more exceptionally than in the South: The area represent51%of all brand-new infections, 8 of the 10 mentions with the greatest rates of brand-new medical diagnoses, and half of all HIV-related deaths, according to the most current information offered from the Centers for Illness Control and Avoidance.
Even prior to the COVID pandemic, Georgia had the greatest rate of brand-new HIV medical diagnoses of any state, though lower than that of Washington, D.C. The Georgia Department of Public Health taped a 70%drop in screening last spring compared to spring 2019.
The downturn in HIV client services “might be felt for years,” stated Dr. Melanie Thompson, primary detective of the AIDS Research Study Consortium of Atlanta.
She included, “Every brand-new HIV infection perpetuates the epidemic and will likely be passed to several individuals in the months to come if individuals are not detected and provided HIV treatment.”
Coronavirus screening has actually commandeered the makers formerly utilized for HIV/AIDS screening, additional straining monitoring efforts. The polymerase domino effect– or PCR– devices utilized to spot and determine the hereditary product in the human immunodeficiency infection are the very same devices that run COVID tests ongoing.
Over the years, as HIV moved inland from seaside cities like San Francisco, Los Angeles and New York City, it settled in the South, where hardship is endemic, absence of health protection is prevalent, and HIV preconception is prevalent.
” There is the preconception that’s genuine. There is tradition bigotry,” stated Dr. Thomas Giordano, medical director of Thomas Street University Hospital in Houston, among the biggest HIV centers in the U.S. The state’s politicians, he stated, view HIV as “an illness of the bad, of Blacks, Latinos and gay. It’s simply not mainstream at the state level.”
Black individuals represent 13%of the U.S. population however about 40%of HIV cases– and deaths. In numerous Southern states, the variations are plain: In Alabama, Black locals represent 27%of the population and 70%of brand-new medical diagnoses; in Georgia, Black individuals comprise 33%of locals and 69%of individuals with HIV
HIV centers that serve low-income clients likewise deal with constraints utilizing video and phone visits. Center directors state bad clients typically do not have information strategies and numerous homeless clients merely do not have phones. They likewise need to compete with worry. “If a pal provided you a space to sleep and your buddy learns you have HIV, you may lose that location to sleep,” stated del Rio of Emory University.
Texting can be difficult, too. “We need to beware about text,” stated Dr. John Carlo, president of PRISM Healthcare North Texas in Dallas. “If somebody sees their phone, it can be ravaging.”
In Mississippi, HIV contact tracing– which was utilized as a design for some regional efforts to track the coronavirus– has actually been restricted by COVID-related travel limitations suggested “to secure both personnel and customer,” stated Melverta Bender, director of the STD/HIV workplace at the Mississippi State Department of Health.
Of all areas in the U.S., the South has the weakest health safeguard. And Southern states have far less resources than states like California and New York City. “Our public health facilities have actually been chronically underfunded and weakened over the years,” stated Thompson, the Atlanta scientist. “So we stand to do even worse by numerous metrics.”
Georgia’s high HIV infection rate and the state’s sluggish rate of COVID vaccinations “are not unassociated,” Thompson stated.
The permeable safeguard reaches medical insurance, a crucial requirement for those coping with HIV. Almost half of Americans without health protection reside in the South, where lots of states have actually not broadened Medicaid under the Affordable Care Act. That leaves many individuals with HIV to depend on the federal Ryan White HIV/AIDS Program and state-run HELP drug help programs, called ADAPs, which provide minimal protection.
” As a matter of equity, insurance coverage is crucial for individuals to live and love HIV,” stated Tim Horn, director of healthcare gain access to at NASTAD, the National Alliance of State and Territorial AIDS Directors. Ryan White and ADAPs “are not geared up to offer that complete sweep of thorough care,” he stated.
Roshan McDaniel, South Carolina’s ADAP program supervisor, states 60%of South Carolinians registered in ADAP would certify if her state broadened Medicaid. “The very first couple of years, we thought of it,” stated McDaniel. “We do not even consider it nowadays.”
Registration in the Ryan White program leapt throughout the early months of the pandemic when state economies froze and Americans hunched down amidst a grinding pandemic. Information from state health departments show the increased requirement. In Texas, registration in the state’s HELP drug program increased 34%from March to December2020 In Georgia, registration leapt by 10%.
State health authorities associate the increased registration to pandemic-related task losses, specifically in states that didn’t broaden Medicaid. Antiretroviral treatment, the recognized program that reduces the quantity of infection in the body and avoids AIDS, costs as much as $36,000 a year, and medication disturbances can result in viral anomalies and drug resistance. Certifying for state support is challenging: Approval can take up to 2 months, and missing out on documents can lead to canceled protection.
Federal health specialists state Southern states have actually typically dragged getting clients into healthcare and reducing their viral loads, and individuals with HIV infections tend to go undiagnosed longer there than in other areas. In Georgia, for instance, almost 1 out of 4 individuals who discovered they were contaminated established HELP within a year, showing their infections had actually long gone undiagnosed.
As vaccinations end up being commonly readily available and constraints ease, HIV center directors are searching their client lists to identify who they require to see. “We are taking a look at the number of individuals have not seen us in over a year. We believe it’s over a number of hundred. Did they move? Did they move companies?” stated Carlo, the medical professional and healthcare CEO in Dallas. “We do not understand what the long-lasting repercussions are going to be.”
No comments:
Post a Comment